Corneal Ulcer: Symptoms, Causes and Treatments
Published on March 26th, 2025
 Australia
Australia
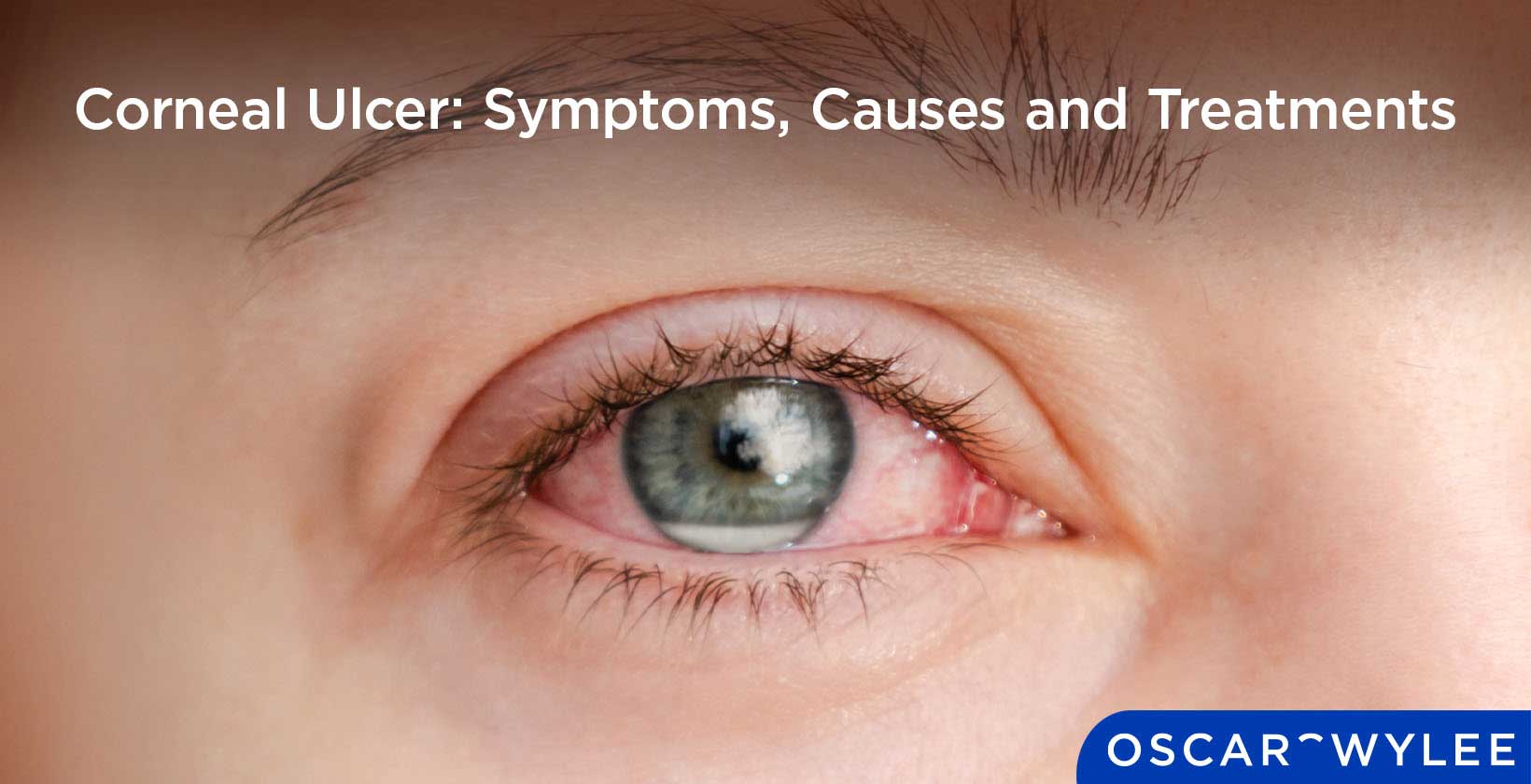
A corneal ulcer refers to an open sore that forms on the surface of the cornea, at the front of the eye. These ulcers can be caused from infections, untreated external injuries, or underlying eye conditions. Left untreated, they can cause potentially significant impacts on your eye health such as scarring, cataracts or even vision loss. Read on for more information on corneal ulcers such as their symptoms, causes and treatments that can be undertaken to heal them.
What is a Corneal Ulcer?
A corneal ulcer is an open sore or lesion on the cornea, which refers to the clear front surface of the eye. It often results from infection or underlying health conditions such as dry eye or excessive contact lens use. The ulcer can impair vision by causing scarring or distortion. If untreated, corneal ulcers may lead to more serious vision problems such as vision loss or deeper infection.
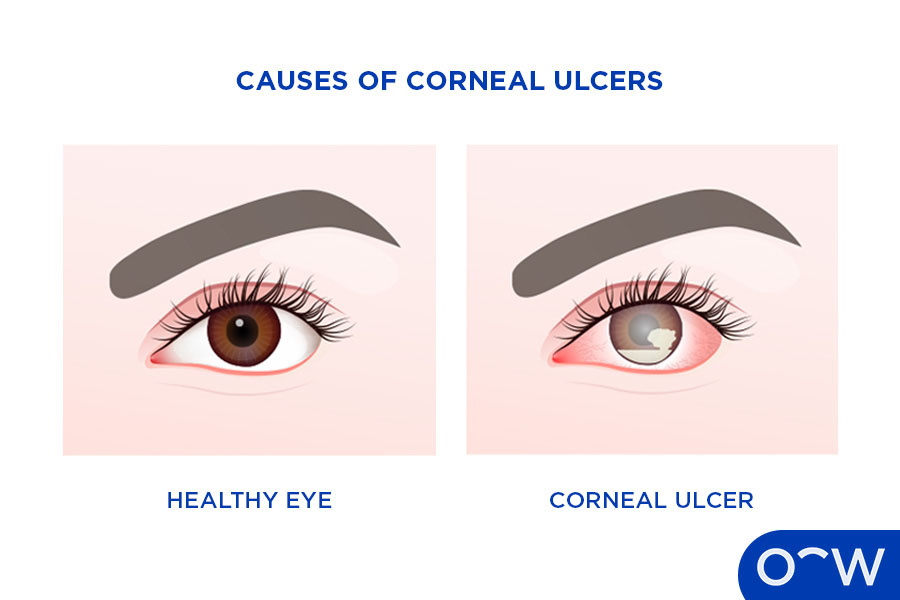
What are the Causes of Corneal Ulcers?
The causes of corneal ulcers can be divided into infectious causes and non-infectious causes, according to the Cleveland Clinic. Infectious causes are conditions that you can catch from or spread to others. Bacteria such as Pseudomonas which affects the cornea, viruses such as herpes, fungal infections and parasites are examples of infectious causes of corneal ulcers. Noninfectious causes can cause corneal ulcers without an infection. Examples of this include eye injuries, dry eyes and autoimmune conditions.
What are Corneal Ulcer Symptoms?
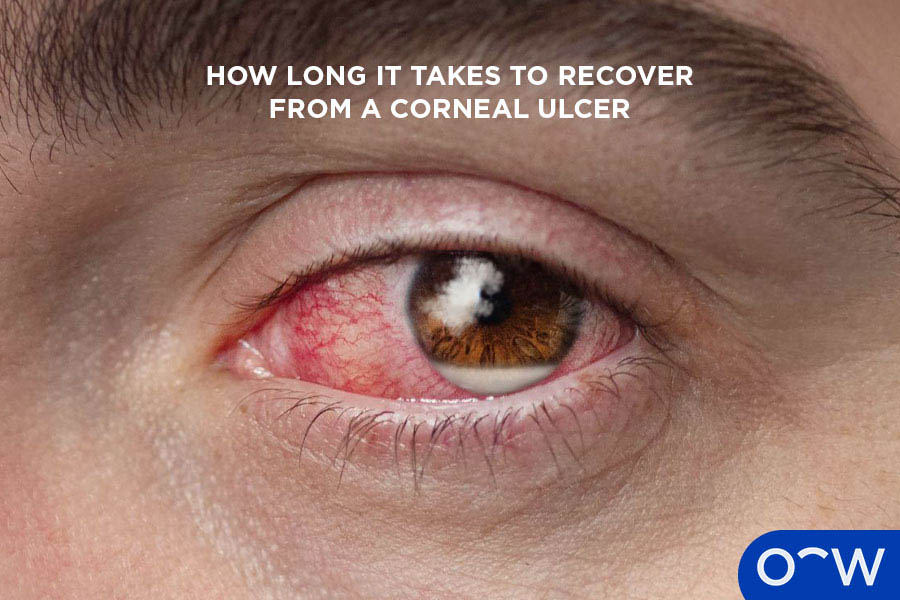
The common symptoms of corneal ulcer include a red, bloodshot, teary or watery eye, varying degrees of eye pain, light sensitivity, blurred vision, feeling like something is stuck in your eye and inflamed or swollen eyelids. However, the symptoms of a corneal ulcer can vary from person to person. Read on for the corneal ulcer symptoms.
- Red, bloodshot, teary or watery eye: Red and bloodshot or teary and watery eyes are a physical symptom of a corneal ulcer.
- Varying degrees of eye pain: There will be varying degrees of eye pain present in corneal ulcers, depending on its severity.
- Light sensitivity: Light sensitivity will emerge as a symptom of corneal ulcer as places with high lighting will prove uncomfortable.
- Blurred vision: Blurred vision is a common symptom of corneal ulcers, as vision becomes less clear when they are present.
- Feeling like something is stuck in your eye: You may feel like something is stuck in your eye like hair or dust when you have a corneal ulcer.
- Inflamed or swollen eyelids: Inflamed or swollen eyelids is another physical symptom of corneal ulcers.
How is a Corneal Ulcer Diagnosed?
According to the Cleveland Clinic, a corneal ulcer is diagnosed by an eye specialist or healthcare provider through an eye exam. A key part of the eye exam that they will do is the slit lamp exam. This examines the inside of the eye to detect signs of eye disease and check overall eye health, looking at a patient’s conjunctiva, sclera, cornea, iris, pupil, lens, retina and optic nerve. Another lab test your provider might do is a swab culture. This involves taking a soft-tipped swab, collecting some of the discharge from your eye and then sending that to a lab for testing. The test results may tell your provider what kind of infection is causing your ulcer. If ineffective, your provider may recommend taking this a step further and do a corneal biopsy which involves taking a sample of your corneal tissue for testing.
What Are Available Corneal Ulcer Treatments?
There are various available corneal ulcer treatments depending on the cause. According to Health Direct, the causes of corneal ulcers include a foreign body present, an infection, or excess use of contact lenses. Upon the diagnosis of a corneal ulcer by an optometrist, the patient may then be referred to an ophthalmologist for the treatment options. Read more on the different treatments for these causes below.
- Foreign body present: A foreign body present in your eye can cause an ulcer. Your doctor will first remove the object and you will be given anti-fungal medicine if the foreign body is organic, and fungal keratitis is present.
- Infection: If an infection is the cause of your ulcer, you will probably be given antibiotic, antiviral or antifungal eye drops as per the doctor’s instruction.
-
What are the Potential Complications of An Untreated Corneal Ulcer?
The potential complications of an untreated corneal ulcer include scarring, glaucoma and even vision loss. Read more below on the potential complications of an untreated corneal ulcer.
- Scarring: Permanent scarring can occur on the cornea, particularly if it is not treated immediately.
- Glaucoma: Glaucoma can occur as a result of an untreated corneal ulcer, which is characterized by increased intraocular pressure that can cause vision loss.
-
Can a Corneal Ulcer Lead to Permanent Vision Loss?
Corneal ulcers can lead to permanent vision loss. According to the Cleveland Clinic, corneal ulcers need immediate care because they can cause permanent eye damage, low vision and even blindness. Early treatment can help minimize this risk, which is why it is important to seek help immediately.
What are the Types of Corneal Ulcer?
The types of corneal ulcers can be differentiated by their causes: bacterial, viral, fungi, or parasitic. Read more about these types of corneal ulcers below.
- Bacterial: Bacterial ulcers occur particularly for people who wear contact lenses. If they are worn for extended periods of time or not regularly cleaned, there is a high risk of a corneal ulcer forming.
- Viral: Viral diseases such as herpes simplex and the herpes zoster virus can be the cause of corneal ulcers.
- Fungal: Fungal infections can emerge as a result from an injury to the cornea that lets plant material get into the eye. It can also occur from the use of steroid eye drops.
-
How Can You Prevent a Corneal Ulcer from Developing?
There are ways you can prevent a corneal ulcer from developing. If you wear contact lenses, it is key to regularly maintain them. Clean and store lenses carefully, wear them the recommended amount, avoid wearing contact lenses overnight, and always wash your hands thoroughly before touching your lenses. You should manage dry eyes using eye drops or other medication recommended by a doctor, and seek prompt help if an infection or changes in your eye develop.
What Role Do Contact Lenses Play in Corneal Ulcer Development?
Unfortunately, contact lenses can play a role in corneal ulcer development due to their proximity to the cornea. According to Health Direct Australia, contact lenses are a risk factor to corneal ulcer development particularly if they are worn while sleeping, worn for longer than recommended, and not handled in a hygienic manner. That is why it is important to regularly clean your contact lenses, and only wear them for the recommended amount of time.
How is a Corneal Ulcer Differentiated from Other Eye Conditions?
Corneal ulcers are differentiated from other eye conditions as they have a specific diagnosis. According to the Australian Journal of General Practice the diagnosis of the corneal ulcer happens when there is corneal abrasion involving the corneal epithelium and stroma, which is the outermost layer of the cornea. However it can extend deeper depending on the severity of the ulcer. Physically your eye will be red or bloodshot, teary, and an optometrist will be able to see a white or gray spot on your cornea under a slit lamp.
What are the Risks of Surgery for Corneal Ulcers
There is a small risk of complications occurring for a cornea transplant, which is the surgery that may be undertaken for severe corneal ulcers. However, complications are still possible and according to Mayo Clinic can include the rejection of the donor cornea, eye infection and glaucoma. Read more about these risks below.
- Rejection of the Donor Cornea: The rejection of the donor cornea is a potential complication of corneal ulcer surgery. The body's immune system can mistakenly attack the donor cornea. This is called rejection. Rejection might require medical treatment or another cornea transplant.
- Eye Infection: Eye infection is a possibility of corneal ulcer surgery which can lead to corneal scarring.
- Glaucoma: Glaucoma is an eye disease that can occur as a result of a surgery complication. It is characterized by increased intraocular pressure that can cause vision loss.
After the procedure, you will be expected to take measures such as medication to control infection, wear eye protection, and return for follow-up exams.
What are the Key Differences Between Corneal Ulcers and Cataracts?
There are key differences between corneal ulcers and cataracts, with corneal ulcers referring to a sore on the cornea and cataracts referring to the clouding of the lens. They are both serious eye conditions that affect different parts of the eye. A corneal ulcer is an open sore on the cornea typically caused by infection, trauma, or underlying disease. It can cause scarring and if untreated, vision loss. Contrastingly a cataract is a clouding of the eye’s lens, usually related to aging or injury, leading to blurry vision and light sensitivity.
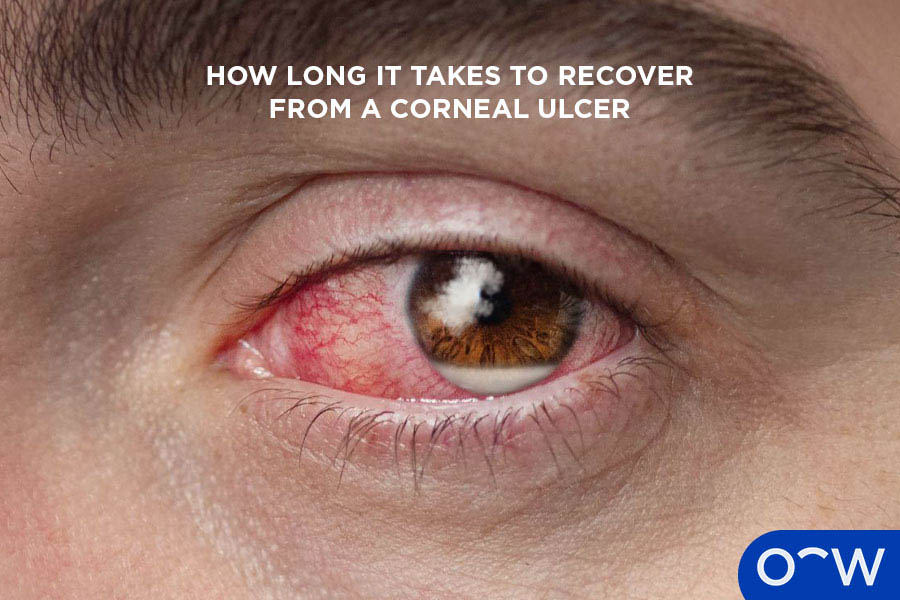
How Long Does It Take to Recover from A Corneal Ulcer?
According to Health Direct, corneal ulcers often improve after 2 or 3 weeks of treatment. However, this can vary on the size of the ulcer and the effectiveness of the medication. Notably, an ulcer in the centre of the eye might take longer to recover from.
What Lifestyle Changes can Help Prevent Corneal Ulcers?
There are lifestyle changes that can help prevent corneal ulcers. Maintain good eye hygiene such as safe handling, storage and cleaning of your contact lenses. Protective eyewear should be worn when doing work or play which can lead to eye injury. Lastly, you should stay on top of taking care of pre-existing eye conditions such as dry eyes by taking medication as recommended by the doctor.
When Should You See a Doctor for Suspected Corneal Ulcers?
You should see a doctor for suspected corneal ulcers when you start to exhibit symptoms. These symptoms include the feeling something is in your eye, swollen eyelids, eye redness and particularly more serious symptoms such as severe eye pain, blurred vision and light sensitivity.
Should I Be Off Work with a Corneal Ulcer?
Taking time off work with a corneal ulcer will likely be the best decision to make. This will allow you to rest your eyes and prevent worsening symptoms, as well as more easily stick to your treatment plan uninterrupted. However, this can depend on the severity of the corneal ulcer as smaller ones may not have a stark impact on your work situation.
Can the Cornea Repair Itself from Ulcer?
Yes, in most cases the cornea can repair itself from an ulcer. However, this can only be done when proper treatment is advised and followed as this will prevent further complications.
Read Corneal Ulcer: Symptoms, Causes and Treatments in other Oscar Wylee regions and their languages.
 Australia
Australia