Keratoconus: Symptoms, Causes, Diagnosis, and Treatments
Keratoconus is defined as an eye condition in which the centre of the cornea thins and becomes cone-shaped. The cornea is the clear layer at the front of the eye that helps people see by bending and focusing light as it enters the eye. The cornea is generally a rounded, dome shape, but when a person has keratoconus, the cornea turns into a cone-shape which can affect how light enters the eye, leading to vision issues. The exact cause of keratoconus is not known, however, there are risk factors that may increase a person’s likelihood of developing the condition such as young age, eye inflammation, family history and rubbing the eyes. The keratoconus symptoms include blurry vision, double vision, frequent eyeglass prescription adjustments, sensitivity to light and halos around light. The treatment for keratoconus is dependent upon how advanced the condition is but can include glasses, contact lenses, corneal cross-linking and a corneal transplant.
What is Keratoconus?
Keratoconus is an eye condition in which the cornea, the clear layer at the front of the eye, thins and becomes cone-shaped. The cornea is the clear window at the front of the eye that helps people to see by bending and focusing light as it enters the eye. A cornea is generally shaped like a dome. If a person has keratoconus, this means that the centre of the cornea has begun to thin. According to Keratoconus Australia, as the cornea thins, normal eye pressure distorts the cornea and causes a cone-shaped bulge. Keratoconus can affect the way that light is focused when it enters the eye and may distort vision, according to Health Direct. Keratoconus commonly starts in puberty and progresses into the 30s, according to John Hopkins Medicine. In summary, the answer to what is keratoconus is an eye condition in which the cornea becomes cone-shaped due to thinning, which may lead to issues with vision.
What is the Other Term for Keratoconus?
There is no other term for the eye condition keratoconus.
Is Keratoconus the Same as Astigmatism?
No, keratoconus is not the same as astigmatism, however, they both affect the same part of the eye, which is the cornea. Keratoconus may also cause astigmatism. Keratoconus is an eye condition in which the cornea thins, which leads to a cone-shaped bulge. Keratoconus may affect the way light enters the eye and focuses, which can distort vision. Astigmatism is an eye condition in which the cornea or lens is misshapen, which can lead to blurry or distorted vision. According to the American Academy of Ophthalmology, keratoconus may cause irregular astigmatism.
What Part of the Eye does Keratoconus Affect?
Keratoconus primarily affects the cornea, the clear layer at the front of the eye. The cornea is the part of the eye that helps people see by bending and focusing light that enters the eye, also known as refraction. According to Sridhar in the article Anatomy of cornea and ocular surface, the cornea makes up two-thirds of the eye’s refractive power. The cornea also helps protect the eye. Keratoconus is an eye condition in which the cornea will begin to thin, leading to the cornea changing from a round, dome shape, to a cone shape. A cone-shaped cornea will not bend or refract light in the same way as the typically round cornea, which can lead to vision issues.


Does Keratoconus Affect Both Eyes?
Yes, keratoconus usually affects both eyes, however, it may be worse or further progressed in one eye. According to Keratoconus Australia, keratoconus is a bilateral condition, meaning it occurs in both eyes. The progression of keratoconus is not usually equal across both eyes however, with one eye often further progressed than the other.
How Common is Keratoconus?
Keratoconus is a common eye condition, with the Centre for Eye Research Australia stating that 1 in every 84 Australians aged 20 have keratoconus. Keratoconus is also one of the most common reasons for corneal transplants in Australia, according to the Centre for Eye Research Australia. Keratoconus is one of the most common forms of corneal ectasia, which refers to eye conditions that cause corneal thinning and subsequent misshaping of the cornea, according to the Boston Children’s Hospital.
Who Commonly has Keratoconus?
Keratoconus is most common among younger people, typically those in their mid-teens to their 30s. Keratoconus is a common eye problem among younger people, with the condition often beginning between 16 and 30 years of age, with progression usually slowing into the 40s, according to Health Direct.
What are the Symptoms of Keratoconus?
The symptoms of keratoconus can include blurry vision, double vision, frequent eyeglass prescription adjustments, sensitivity to light and halos around light. According to the American Optometric Association, symptoms such as blurry vision and sensitivity to light may first begin to appear in the late teens and 20s, progressing until the 40s. The symptoms of keratoconus are listed below.
- Blurry vision: Blurry vision is a possible symptom of keratoconus, as the change in cornea shape from a dome to a cone, can affect the cornea’s refractive abilities.
- Double vision: Double vision can be a symptom of keratoconus, caused by the misshapen cornea and its ability to refract light properly.
- Frequent eyeglass prescription adjustments: Frequently needing adjustments to a glasses prescription is one of the most common symptoms of keratoconus caused by the changing shape of the cornea.
- Sensitivity to light: Sensitivity to light is a possible symptom of keratoconus caused by the misshaping of the cornea affecting its refracting abilities.
- Halos around lights: Halos around light can be a symptom of keratoconus as the cornea's changing shape can affect how light is received by the eye.
1. Blurry Vision
Blurry vision is one of the earliest and most common symptoms of keratoconus, caused by the changing of the cornea to a cone shape. The cornea is the clear part of the front of the eye that helps us see by bending and focusing light as it enters the eye, known as refraction. If a person has keratoconus, the cornea begins to thin in the centre, and the shape changes from a round, dome shape to a cone shape. The change in the shape of the cornea can affect how light is refracted, leading to blurry vision.
2. Double Vision
Double vision, also known as diplopia, may be a symptom of keratoconus caused by the distorted shape of the cornea. Double vision, or diplopia, refers to seeing two images of the same object, according to the Cleveland Clinic. Keratoconus occurs when the cornea thins and becomes cone-shaped, as opposed to a normal dome or round shape. The cornea is the clear layer at the front of the eye that refracts light and helps us to see. A misshapen cornea caused by keratoconus can affect how light is refracted when it enters the eye, which can result in seeing two images of the same thing, or double vision.
3. Frequent Eyeglass Prescription Adjustments
Frequent eyeglass prescription adjustments are a common symptom among those with keratoconus, caused by the changing shape of the cornea. An optometrist provides a glasses prescription after an eye test, which will contain the information on what glasses or contact lenses a person will need to help correct any vision issues. A glasses prescription will include information such as SPH (Sphere) indicating how near or farsighted a person is, CYL (Cylinder) representing how much astigmatism someone has and PD (Pupillary Distance) referring to the distance between the pupils in a person’s eyes. If a person has keratoconus, they may have frequent adjustments to their glasses prescription as the cornea changes shape, which can affect levels of near or farsightedness and astigmatism.
4. Sensitivity to Light
Sensitivity to light or photophobia can be a symptom of keratoconus, caused by the changing shape of the cornea. Sensitivity to light refers to a feeling of discomfort when the eyes are exposed to light. The thinning of the cornea and its change to a cone shape can affect how light is received by the eye which can lead to sensitivity to light.
5. Halos or Glare Around Lights
Halos around lights can be a symptom of keratoconus. Halos around lights refers to seeing round rings of light around light sources. Halos around light can be a symptom of keratoconus due to the way the cornea becomes cone-shaped as it can affect how light enters the eye. Halos around lights can make seeing at night and completing activities such as night driving difficult, according to Health Direct.
What are the Causes and Risk Factors of Keratoconus?
The exact cause of keratoconus is unknown, however, there are some hereditary and environmental factors that may increase the risk of developing keratoconus including young age, eye inflammation, family history and rubbing the eyes. The risk factors for keratoconus are listed below.
- Young age: Young age is a risk factor for keratoconus as this condition generally begins to develop in the teenage years, from 16 up to 30.
- Eye inflammation: Eye inflammation from conditions such as allergies can heighten the risk of keratoconus as it can damage corneal tissue.
- Family history: People with a family history of keratoconus are at higher risk of developing this eye condition.
- Rubbing the eyes: Rubbing the eyes can lead to a higher risk of keratoconus as it can damage the cornea.
1. Young Age
Young age is a risk factor for keratoconus as this condition most commonly begins to develop in teenagers, as opposed to adults. According to the Centre for Eye Research Australia, keratoconus generally develops from 16 to 30 years of age before stabilising in middle age.
2. Eye Inflammation
Frequent eye inflammation can be a risk factor for keratoconus as the corneal tissue may be damaged, leading to a higher likelihood of developing this condition. Eye inflammation refers to the eye being red, irritated, swollen or itchy and can be caused by conditions such as allergies, eye infections or irritants. Frequent eye inflammation may lead to an increased risk of keratoconus as inflammation can damage corneal tissue, according to John Hopkins Medicine. Allergic conditions that may heighten the risk of keratoconus include eczema and asthma according to Health Direct.
3. Family History
People with a family history of keratoconus are at a higher risk for developing the condition. The American Optometric Association states that 1 in 10 people with keratoconus have a close relative with the condition. Whilst not everyone who has keratoconus has a family history of the condition, it is likely to have one, according to the Centre for Eye Research Australia.
4. Rubbing the Eyes
Excessive rubbing of the eyes, especially during childhood, is a risk factor for the development of keratoconus. Excessive rubbing of the eye can damage the cornea, which may lead to an increased risk of developing keratoconus. Rubbing the eyes refers to using the hands to scrub or put pressure on the eye in a back-or-forth motion. People of all ages may rub their eyes, but it is a habit of most concern in children. Children may rub their eyes if they are tired, or have eye fatigue or eye irritation. According to the Centre for Eye Research Australia, eye rubbing can break down fibres in the cornea, which can contribute to keratoconus.
How is Keratoconus Diagnosed?
Keratoconus is diagnosed by an eye care professional, such as an optometrist or ophthalmologist during an eye test, using diagnostic tools such as a slit-lamp test, corneal topography and pachymetry test. Keratoconus is not always easily diagnosable in its early stages, according to the Centre for Eye Research Australia, as symptoms can resemble other eye conditions. It is important to see an optometrist if you notice your vision changing so that they can perform an eye test and detect conditions like keratoconus early.
What to Expect During Keratoconus Diagnosis?
During a keratoconus diagnosis, you can expect to be asked about your medical history, eye health history and family history. An eye care professional will then conduct an eye test. If keratoconus is suspected, more specific tests may be performed such as a slit-lamp test, corneal topography and a pachymetry test. If you have keratoconus, an eye care professional may refer you to an ophthalmologist so full diagnosis and treatment can be sought.
How Long Does Diagnosis for Keratoconus Take?
The length of time for a keratoconus diagnosis is dependent upon the individual optometrist, the patient and the progression of the keratoconus. Early keratoconus may be hard to detect due to its similarity to other eye conditions and therefore may take longer to diagnose than if the condition is further along with more obvious symptoms. A general routine eye test will typically take 20-30 minutes, however, if keratoconus is suspected, it may take longer for specialised tests.
How Serious is Keratoconus?
Keratoconus can be a serious eye condition as it may lead to decreased vision if left untreated. According to Nebraska Medicine, keratoconus will not lead to blindness. However, keratoconus can lead to blurry vision and other visual problems such as a sensitivity to light if left untreated, which can impact someone’s quality of life. Keratoconus will often need to be treated using glasses, contact lenses or eye surgery in advanced cases.
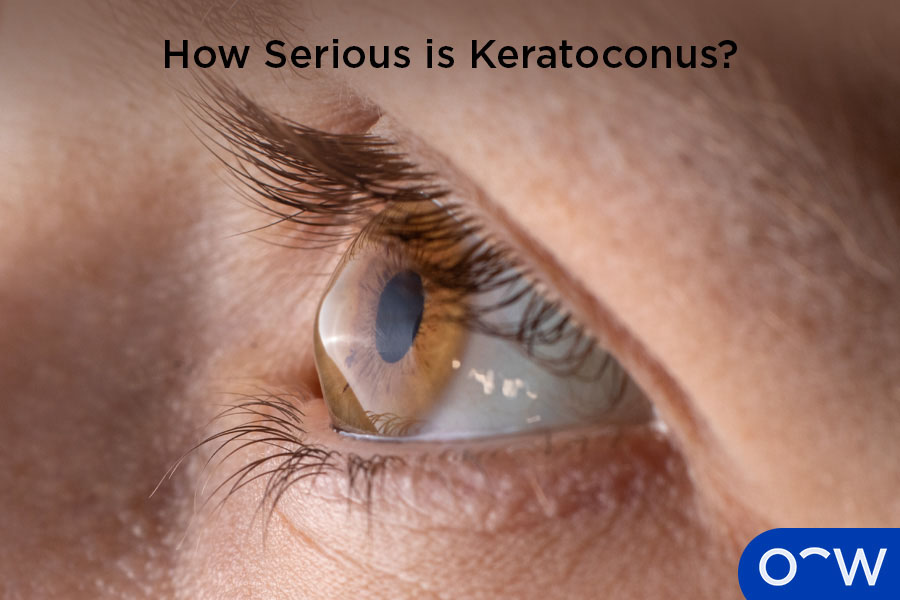
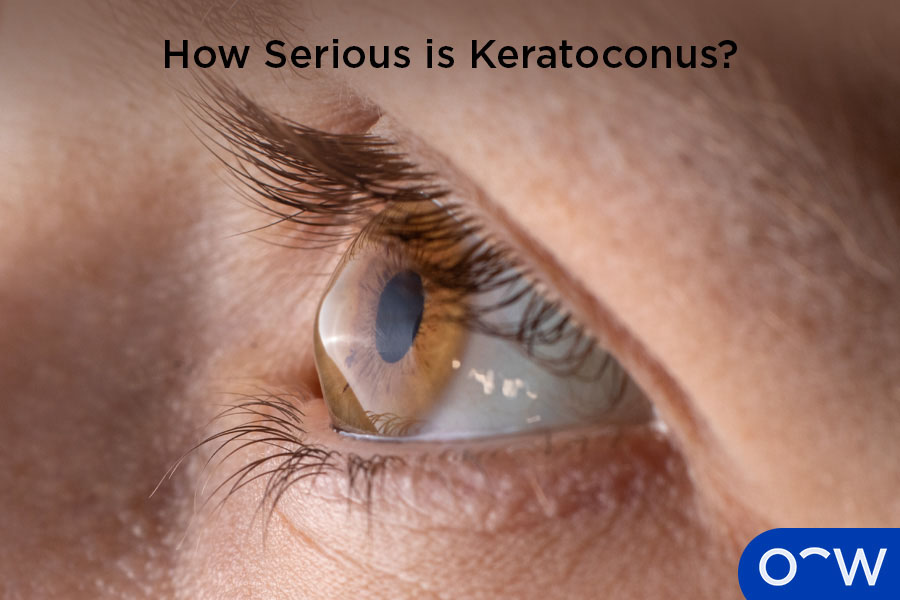
Does Keratoconus Lead to Blindness?
Keratoconus does not generally lead to blindness, but it can cause permanent vision loss if left untreated, according to the Cleveland Clinic. Keratoconus refers to a thinning of the centre of the cornea which leads to the cornea becoming cone-shaped, as opposed to the usual dome or round shape. A misshapen cornea can lead to visual issues and impairments such as blurry vision, reduced vision, sensitivity to light and seeing halos around lights, but will not generally cause a person to go blind. It is important to see an optometrist regularly so they can diagnose and treat eye conditions including keratoconus if present.
Is Keratoconus an Infection or Disease?
Keratoconus is an eye disease that affects the cornea part of the eye. Keratoconus is not an infection, it is an issue with the structures within the eye, with risk factors for the condition related to genetic and environmental factors.
What are the Treatments for Keratoconus?
The main treatments for keratoconus are glasses, contact lenses, corneal cross-linking and a corneal transplant. The exact treatment for keratoconus will be dependent upon the individual and how far their keratoconus has progressed. The treatments for keratoconus are listed below.
- Glasses: Glasses are a type of eyewear designed to help correct vision issues such as myopia, hyperopia and astigmatism. Glasses can be used to help treat keratoconus as the condition commonly affects vision, causing issues such as blurriness. Glasses can help correct vision issues caused by keratoconus and help people see better.
- Contact lenses: Contact lenses are lenses placed on the surface of the eye that have a prescription or power that can help correct vision. Contact lenses may be used in the treatment of keratoconus by helping to correct vision issues such as blurriness, caused by the condition. Hard contact lenses can also be used in the treatment of keratoconus to help keep the cornea in shape.
- Corneal cross-linking: Corneal cross-linking is the process of strengthening the cornea by putting vitamin B12 eye drops in the eye, and then using ultraviolet light on the eye, according to Health Direct. Corneal cross-linking may be used in the treatment of keratoconus if the condition is worsening.
- Corneal transplant: A corneal transplant involves removing the damaged part of a cornea and replacing it with a cornea from a donor. Corneal transplants may be used for keratoconus in advanced cases.
How Long Can Keratoconus Take to Heal?
Keratoconus is not a condition that will heal with treatment unless the treatment is a corneal transplant. Generally, keratoconus treatment focuses on correcting vision issues that arise as a result of the condition by using glasses or contact lenses. Other treatment for keratoconus includes using corneal cross-linking to help strengthen the cornea. The healing time for a corneal transplant, which is used in advanced cases of keratoconus, can be from a few weeks to a few months. According to the NHS, it can take weeks, up to a year for vision to improve after a corneal transplant.
Does Keratoconus Go Away on its Own?
No, keratoconus will not go away on its own, rather it is a disease that affects a person for life. While it can be treated, there is no cure for keratoconus and it cannot be reversed. Treatments for keratoconus include glasses and contact lenses, corneal transplant surgery and corneal cross-linking.
When to call a Doctor about Keratoconus?
If you suspect you have a vision issue such as keratoconus, you can call a doctor, who will likely recommend you see an optometrist or ophthalmologist for further diagnosis and treatment. An eye care professional will be able to conduct an eye test to assess vision and examine the cornea, to assess whether you have keratoconus.
How can Glasses Help Treat Keratoconus?
Glasses, as well as contact lenses, can help treat blurry vision caused by keratoconus in its early stages. Keratoconus is characterised by a thinning of the cornea that leads to the cornea becoming cone-shaped, as opposed to the round, dome shape it usually is. A cone-shaped cornea can change how light enters and is refracted in the eye, which can lead to vision issues such as blurriness. Glasses and contact lenses can help the light refract properly within the eye, and assist with seeing clearer.