Keratoconjunctivitis: Types, Symptoms, Causes, Diagnosis, and Treatments
Published on September 19th, 2024
Keratoconjunctivitis refers to the inflammation of both the conjunctiva and cornea, which can stem from causes such as bacteria, viruses, allergens and pollutants according to the Cleveland Clinic. Keratoconjunctivitis symptoms can include watery eyes, itchy eyes, redness, swollen eyes and discharge. The conjunctiva is defined as the clear tissue that covers the sclera (the white part of the eye) and lines the inside of the eyelid, providing protection for the eyes. The cornea is the clear outer layer of the eye covering the iris and the pupil. Keratoconjunctivitis can occur in non-infectious cases which can lead to allergic keratoconjunctivitis, exposure keratoconjunctivitis and keratoconjunctivitis sicca. Infectious cases of keratoconjunctivitis can include epidemic keratoconjunctivitis, bacterial keratoconjunctivitis, phlyctenular and keratoconjunctivitis, Keep reading to learn more about the symptoms and causes of keratoconjunctivitis, treatment and prevention.
What is Keratoconjunctivitis?
Keratoconjunctivitis is a condition that causes inflammation in the conjunctiva and cornea. Keratoconjunctivitis can develop as a result of viral and bacterial infections, allergic reactions, eye injuries, dry eyes and from pollutants entering the eye. While keratitis and conjunctivitis are separate eye problems, keratoconjunctivitis is when you have both according to the Cleveland Clinic. Symptoms that are commonly associated with keratoconjunctivitis can involve watery eyes, redness, itchy eyes, swelling and discharge.
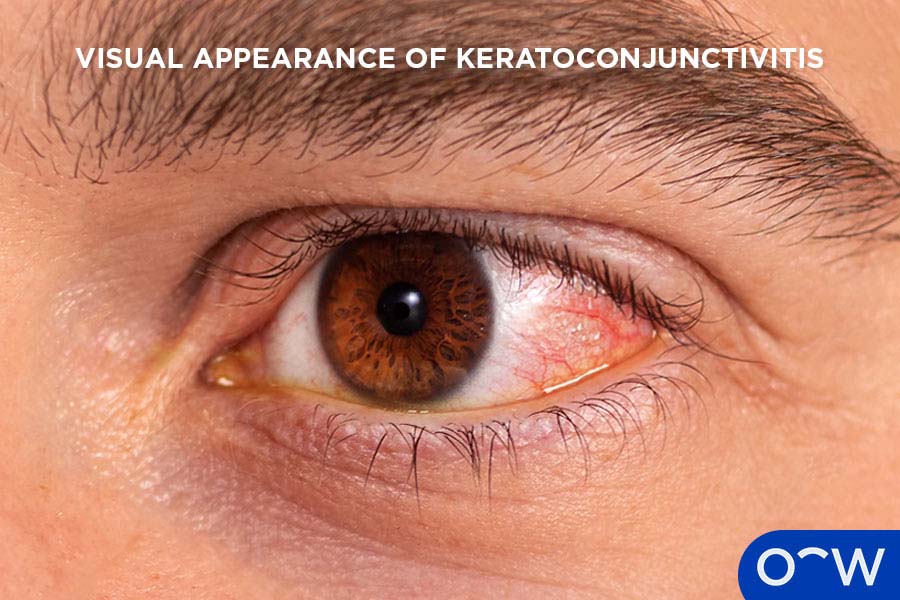
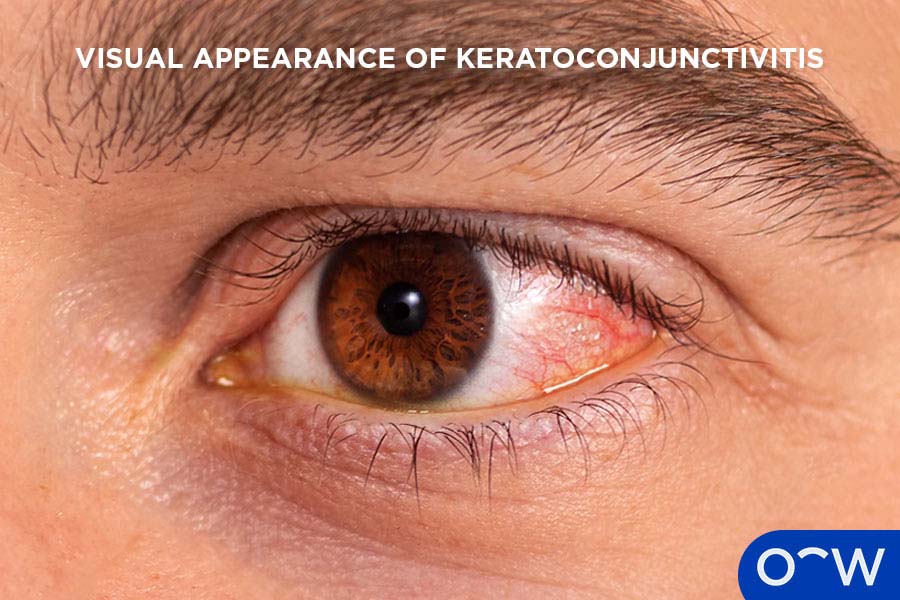
What Does Keratoconjunctivitis Look Like?
Keratoconjunctivitis looks like watery eyes, swollen eyes, discharge filled eyes and redness in the white part of the eye. Individuals with keratoconjunctivitis may not experience all known symptoms as it can depend on the severity of your condition.
The image below depicts what keratoconjunctivitis can look like in affected individuals. The eye pictured below exhibits slight redness, discharge and swelling.
What is the Medical Term for Keratoconjunctivitis?
The medical term for Keratoconjunctivitis is keratoconjunctivitis. This medical term describes inflammation of the cornea and conjunctiva.
Is Keratoconjunctivitis the Same as Dry Eyes?
No, keratoconjunctivitis is not the same as dry eye, however, keratoconjunctivitis can develop as a consequence of dry eye. Dry eyes can mean that the eyes are not producing enough tears to maintain optimal moisture. The other cause for dry eyes can be that the tears that are produced, are evaporating too quickly causing dryness in the eyes. Keratoconjunctivitis that is caused by dry eyes is referred to as keratoconjunctivitis sicca according to the College of Optometrists.
How Common is Keratoconjunctivitis?
Keratoconjunctivitis can be common depending on the type of this condition. A common form of keratoconjunctivitis may be allergic keratoconjunctivitis according to the Cleveland Clinic. Up to 40% of the population are affected by allergic keratoconjunctivitis according to Baab, Le, Gurnani and Kinzer (2024).
Is Keratoconjunctivitis a Common Disease on the Cornea?
No, it may not be considered a common disease on the cornea, however, forms such as allergic conjunctivitis is considered common. Other common diseases on the cornea can include keratitis, corneal ectasia and corneal dystrophy according to the Cleveland Clinic.
Who Typically Gets Keratoconjunctivitis?
Anyone can get keratoconjunctivitis as it can develop through various causes. However, certain groups of people may be more susceptible to certain forms of keratoconjunctivitis. Vernal keratoconjunctivitis is an allergy associated form that is reported to affect young males living in hot climates according to Burrow and Patel (2023). Children are most commonly associated with allergic, viral and bacterial keratoconjunctivitis according to the Cleveland Clinic.
Do Children Get Keratoconjunctivitis?
Yes, children can get keratoconjunctivitis. Children may be more likely to contract viral and bacterial keratoconjunctivitis and allergic conjunctivitis according to the Cleveland Clinic. Children may be more vulnerable to viral and bacterial forms of keratoconjunctivitis due to their developing immune systems and smaller anatomy. Children’s higher chances of getting allergy-associated keratoconjunctivitis are a result of their underdeveloped mucosal defences according to the National Institutes of Health.


What are the Different Types of Keratoconjunctivitis?
The different types of keratoconjunctivitis include vernal keratoconjunctivitis, epidemic keratoconjunctivitis, atopic keratoconjunctivitis, superior limbic keratoconjunctivitis, allergic keratoconjunctivitis, keratoconjunctivitis sicca and phlyctenular keratoconjunctivitis. It is important to note that keratoconjunctivitis symptoms of redness, itchy eyes, swelling, watery eyes and discharge are typically similar across the different forms. The different types of keratoconjunctivitis are listed below.
- Vernal Keratoconjunctivitis: Vernal keratoconjunctivitis is a recurrent form that occurs from allergic reactions and can affect both eyes.
- Epidemic Keratoconjunctivitis: Epidemic keratoconjunctivitis is categorised as a form of viral keratoconjunctivitis and is highly contagious.
- Atopic Keratoconjunctivitis: Atopic keratoconjunctivitis is a chronic, allergy associated form of keratoconjunctivitis that develops in patients with atopic dermatitis.
- Superior Limbic Keratoconjunctivitis: Superior limbic keratoconjunctivitis is a rare form of keratoconjunctivitis and causes inflammation in the superior bulbar conjunctiva, limbus and upper cornea.
- Allergic Keratoconjunctivitis: Allergic keratoconjunctivitis is a form that ensues when coming into contact with allergens such as pet dander, pollen and dust.
- Keratoconjunctivitis Sicca: Keratoconjunctivitis sicca can develop as a consequence of dry eyes.
- Phlyctenular Keratoconjunctivitis: Phlyctenular keratoconjunctivitis causes an immune reaction to bacteria that is on or around the eyes.
1. Vernal Keratoconjunctivitis
Vernal keratoconjunctivitis is a recurrent allergic disorder that typically occurs during spring or warm weather. Vernal keratoconjunctivitis is considered non-contagious and is often found in patients with atopic dermatitis or eczema according to the College of Optometrists. This form of keratoconjunctivitis typically affects young male patients within the age range of 3-25 years old according to the National Organisation for Rare Disorders.
2. Epidemic Keratoconjunctivitis
Epidemic keratoconjunctivitis also referred to as viral keratoconjunctivitis is a very contagious form that is caused by adenoviruses. Epidemic keratoconjunctivitis can be spread by coming into contact with an infected person’s tears or discharge from their eyes and then touching your own eyes. This may occur when touching surfaces that may be contaminated or touching an infected person’s hands. According to NSW Health, there is no treatment for epidemic keratoconjunctivitis and should alleviate on its own after 1 to 6 weeks.
3. Atopic Keratoconjunctivitis
Atopic keratoconjunctivitis is chronic and affects patients with atopic dermatitis. According to the University of Michigan Health, this form can occur all year round but may worsen during winter. Atopic keratoconjunctivitis may affect the lower eyelid more than the upper eyelid, which can help differentiate from vernal keratoconjunctivitis. A combination of topical and oral antihistamines may be helpful in managing symptoms according to the University of Michigan Health.
4. Superior Limbic Keratoconjunctivitis
Superior limbic keratoconjunctivitis is the inflammation of superior bulbar conjunctiva, limbus and upper cornea. Superior limbic keratoconjunctivitis may be related to keratoconjunctivitis sicca, thyroid dysfunction and rheumatoid arthritis according to Bert et al. (2024). This form of keratoconjunctivitis has been noted to affect women in their 60s more than men according to the American Academy of Ophthalmology and may require different types of topical steroids for treatment. However, there is not enough robust evidence to confirm the most effective treatment.
5. Allergic Keratoconjunctivitis
Allergic keratoconjunctivitis is a very common form that can occur when coming into contact with allergens such as animal dander, pollen and dust. Allergic keratoconjunctivitis may only arise among individuals who do experience allergic reactions to certain substances. According to the National Institutes of Health, antihistamine eye drops prescribed from an optometrist may help alleviate symptoms.
6. Keratoconjunctivitis Sicca
Keratoconjunctivitis sicca refers to the inflammation of the cornea and conjunctiva as a result of dry eyes. Keratoconjunctivitis sicca may come about when the eyes are not able to generate enough tears or when the eyes produce tears that evaporate too quickly. This can lead to a lack of proper moisture in the eyes causing dryness, irritation and discomfort. Applying artificial or lubricating tears every couple of hours can typically reduce the problem. Artificial tears are eye drops mixed with substances that mimic real tears and assist with keeping the eyes coated with moisture.
7. Phlyctenular Keratoconjunctivitis
Phlyctenular keratoconjunctivitis may be associated with hypersensitivity reactions as a consequence of Mycobacterium tuberculosis or chlamydial infections. However, it can also originate from other bacterial, viral, or environmental allergens. Treatment may require addressing the initial cause, such as antimicrobial treatment for infections, corticosteroids to reduce inflammation and relieve symptoms. Lubricating eye drops or artificial tears may also be recommended to reduce dryness and discomfort. It is important to see an optometrist so you can receive a professional diagnosis and the right form of treatment.
What are the Symptoms of Keratoconjunctivitis?
The symptoms of keratoconjunctivitis include eye discharge, feeling something in your eye, swollen eyelids (blepharitis), burning in the eye, light sensitivity (photophobia), watery eyes, itchy eyes and redness in the eyes. The symptoms of keratoconjunctivitis are listed below.
- Eye Discharge: Eye discharge is the clear, grey, or in some cases yellowish mucus-like substance that is released from the eye when experiencing eye injuries, infections and dryness.
- Feeling something in your eye: Feeling something in your eye is a symptom of keratoconjunctivitis can stem from the dryness, injuries and infections that occur.
- Swollen Eyelids (Blepharitis): Swollen eyelids (blepharitis) are when the eyelids become puffy and slightly red as a natural reaction to inflammation.
- Burning in the eye: Burning in the eye may feel like a stinging sensation, which occurs when the eyes lack moisture or when they become irritated.
- Light Sensitivity (Photophobia): Light sensitivity (photophobia) is defined as feeling discomfort or the inability to keep eyes open normally when the eyes are exposed to bright lights.
- Watery Eyes: Watery eyes are characterised by the increased production of tears in response to dryness, injuries and infections.
- Itchy Eyes: Itchy eyes are a symptom of keratoconjunctivitis that arises during an allergic reaction and infections.
- Redness in the eyes: Redness in the eyes occurs when the small vessels under the surface of the eyes become larger in response to inflammation.
1. Eye Discharge
Eye discharge is a typical symptom of keratoconjunctivitis as a result of injuries, infections, dryness and allergies. Eye discharge is characterised as a clear, grey or yellowish, mucus-like fluid that can be found in the eyes. Eye discharge can typically develop when inflammation arises in the eye causing the eyes to create more mucus resulting in eye discharge as the eye’s attempt to remove irritants or debris.
2. Feeling something in your eye
Feeling something in your eye can be another common attribute of keratoconjunctivitis due to inflammation symptoms. It can easily feel like something is in your eye due to increased sensitivity and irritation of the eye's surface. The inflammatory response can also affect certain nerves of the eye, making the eye more sensitive to discomfort.
3. Swollen Eyelids (Blepharitis)
Swollen eyelids (blepharitis) are a symptom of keratoconjunctivitis that is characterised by the increased and puffy appearance of the eyelids and slight redness. Swollen eyelids or blepharitis can occur during inflammation, triggering more white blood cells and fluids to flow towards the affected or injured area. This is part of the body’s healing process and is what contributes to the swollen and slightly red appearance of the eyelids according to the National Institutes of Health.
4. Burning in the eye
Burning in the eye can feel similar to a stinging sensation and generally occurs when the eyes are dry or irritated. The burning feeling in the eyes can take place during keratoconjunctivitis as the tissues of the eye increase in sensitivity and typically occurs along with other common inflammation symptoms.
5. Light Sensitivity (Photophobia)
Light sensitivity (photophobia) can arise during keratoconjunctivitis as the eyes are more susceptible to discomfort. The eyes can become more sensitive when exposed to stimuli such as bright lights according to the National Institutes of Health. Light sensitivity may be alleviated when the initial cause is addressed, however, it may be helpful to wear sunglasses or avoid the use of bright artificial light.
6. Watery Eyes
Watery eyes are a common symptom of keratoconjunctivitis and can occur from dryness, infections and injuries. Watery eyes develop during keratoconjunctivitis as a way for the eye to eliminate whatever may be causing the issue in the eye. It is also how the eye maintains optimal moisture for comfort and health.
7. Itchy Eyes
Itchy eyes may come about when experiencing keratoconjunctivitis as a result of allergies and infections. The itchy sensation occurs when the body releases histamine, a chemical that produces allergic reaction symptoms. Infections may also lead to itchy eyes poor also as part of the body’s immune response to bacteria and viruses getting into the eye according to Science Direct.
8. Redness in the eyes
Redness in the eyes may develop when experiencing keratoconjunctivitis as a result of the inflammation. Redness in the eyes can develop due to the dilation of small blood vessels that are in the white of the eye which causes the red appearance of the eyes. When the eyes are injured, the eyes can become dilated, bringing the blood cells to the affected area to repair and heal the injury.
What are the Causes of Keratoconjunctivitis?
The causes of keratoconjunctivitis are autoimmune disorders, bacteria, viruses, allergens and pollutants. The causes of keratoconjunctivitis are listed below.
- Autoimmune Disorders: Autoimmune disorders cause a patient’s immune system to attack the body and may be a cause of keratoconjunctivitis.
- Bacteria: Bacteria can be a common cause of keratoconjunctivitis as certain types of bacteria can contaminate the cornea and conjunctiva.
- Viruses: Viruses such as adenovirus can remain on surfaces for up to 30 days making it easy to come into contact with and contract keratoconjunctivitis.
- Allergens: Allergens may cause keratoconjunctivitis for individuals who may be allergic to certain substances such as pollen, mould, dust and animal dander.
- Pollutants: Pollutants can get into the eye and cause injury or irritation, which can result in keratoconjunctivitis depending on the type of pollutant.
1. Autoimmune Disorders
Autoimmune disorders can be a possible risk factor for developing keratoconjunctivitis due to their compromised or poor immune systems. Autoimmune disorders refer to when a patient’s immune system attacks their own body as it fails to distinguish between healthy tissues and potentially harmful substances. This leads to the body initiating a reaction that harms normal tissues according to MedlinePlus.
2. Bacteria
Bacteria is one of the most common causes of keratoconjunctivitis as bacteria can easily get into the eye causing contamination. Bacteria can develop as a result of poor hygiene or touching your eyes after touching contaminated surfaces and is typically common in children according to the Cleveland Clinic.
3. Viruses
Viruses are also a very common cause in developing keratoconjunctivitis as they are highly contagious and easy to come into contact with, from an infected individual. This may occur by touching their eye discharge or tears from contaminated surfaces or their hands and then touching your eyes.
4. Allergens
Allergens are a typical cause of keratoconjunctivitis as pollen, mould, dust and pet dander can trigger the body’s inflammation system. Individuals with allergies may have a higher chance at developing keratoconjunctivitis than those who do not have existing allergies to those substances. Keratoconjunctivitis that is caused by allergens may be alleviated with antihistamine eye drops prescribed by an optometrist.
5. Pollutants
Pollutants can likely contribute as a risk factor for keratoconjunctivitis as they can irritate or burn the surface of the eye. Pollutants in the air can include particulate matter, nitrogen oxides and carbon dioxides according to the National Library of medicine. The effects of particulate matter, nitrogen oxides and carbon oxides are found to irritate the eyes and least to inflammation according to a 2022 study on The Adverse Effects of Air Pollution on the Eye: A Review.
How is Keratoconjunctivitis Diagnosed?
Keratoconjunctivitis is diagnosed through an eye test with an optometrist. The optometrist may ask about your medical history and assess the symptoms you are experiencing. As part of the standard eye test, a visual acuity test is carried out to check your vision and a slit-lamp examination to evaluate if there is inflammation in the cornea and conjunctiva.
What are the Eye Tests For Keratoconjunctivitis?
A normal eye test will be carried out for keratoconjunctivitis and will therefore include a visual acuity test and a slit-lamp examination. It is important to have an eye test for keratoconjunctivitis with an optometrist first as they can refer you to a specialist if necessary. Other eye tests that may be required to diagnose your condition include a lacrimal function test and a cornea sensitivity test, however, these will be conducted by an ophthalmologist. Depending on the cause and severity of your condition, you may be directed to an ophthalmologist for further examination. The eye tests for keratoconjunctivitis are listed below.
- Visual Acuity Test: A visual acuity test can help diagnose keratoconjunctivitis and confirm how sharp your vision is. This test will involve reading different sized letters from a chart while standing at standard distance according to the National Institutes of Health.
- Slit-Lamp Examination: A slit-lamp examination helps to assess the structures of the eye with the use of a special magnifying microscope.
- Lacrimal Function Test: A lacrimal function test can assist with seeing whether the eyes produce enough tears to maintain moisture.
- Cornea Sensitivity Test: A cornea sensitivity test can be used to check for keratoconjunctivitis as it can confirm whether your normal blink reflex has been compromised.
How Dangerous is Keratoconjunctivitis?
Keratoconjunctivitis may be dangerous in certain cases and when left untreated, however, it may also not be considered dangerous depending on its initial cause. Keratoconjunctivitis can range from mild to severe with viral and allergic forms typically being less serious and may alleviate on their own. However cases like bacterial keratoconjunctivitis, can lead to complications such as corneal scarring or vision loss, if left untreated. Chronic or severe cases may require medical treatment to prevent prolonged discomfort or eye damage.
Does Keratoconjunctivitis Lead to Blindness?
Yes, keratoconjunctivitis can lead to blindness, however, this may only occur in more severe cases and depend on the initial cause. Certain types of keratoconjunctivitis such as vernal keratoconjunctivitis can lead to vision loss if no treatment is sought according to the American Academy of Paediatrics.
What are the Treatments for Keratoconjunctivitis?
The treatment for keratoconjunctivitis may be artificial tears, antihistamine eye drops and antibiotic eye drops prescribed by an optometrist. However, this will depend on your condition and the underlying cause. The treatments for keratoconjunctivitis are listed below.
- Artificial Tear Drops: Artificial tear drops can help with restoring moisture or maintaining moisture in the eyes during keratoconjunctivitis.
- Antibiotic Eye Drops: Antibiotic eye drops may aid with bacterial infections that can lead to keratoconjunctivitis.
- Antihistamine Eye Drops: Antihistamine eye drops can alleviate allergic reaction symptoms such as itchiness, redness and swelling.
What Type of Eye Drops Help Treat Keratoconjunctivitis?
The type of eye drops that help treat keratoconjunctivitis can include antibiotic eye drops, antihistamine eye drops and artificial tears. However, these may not be able to treat all types of keratoconjunctivitis. It is important to see your optometrist so you can get a professional examination so they can also advise what type of eye drops to use and if any other medication is required.
How Long Does Keratoconjunctivitis Last?
Keratoconjunctivitis can last up to two or three weeks. However, more serious types may differ and can depend on the initial cause. According to NSW Health, epidemic keratoconjunctivitis can last up to two weeks or more and symptoms from vernal keratoconjunctivitis can last between 7 and 21 days according to the National Institutes of Health.
Does Keratoconjunctivitis Heal Overnight?
No, keratoconjunctivitis does not heal overnight. Keratoconjunctivitis usually takes at least a week or more to fully recover. According to the Cleveland Clinic, keratoconjunctivitis can be hyperacute which means that it lasts less than 1 week, acute cases last 3 to 4 weeks and chronic cases can last more than 4 weeks.
How to Prevent Keratoconjunctivitis?
To prevent keratoconjunctivitis, wash your hands regularly, take allergy medications and manage sugar levels. It may not be easy to prevent all types of conjunctivitis as some cases can happen from a variety of factors or unknown causes. It is always advised to see an optometrist or your GP so you can get professional advice. The steps to prevent keratoconjunctivitis are listed below.
- Wash Your Hands Regularly: Wash your hands regularly to avoid spreading viruses or bacteria that can result in keratoconjunctivitis. It is important to wash your hands for at least 20 seconds to ensure proper removal of any germs you may have picked up from touching different surfaces according to the Centers for Disease Control and Prevention.
- Take Allergy Medication: Take allergy medication, if you do have existing allergies or you can speak with your GP about identifying possible allergies through an allergy test.
- Manage Sugar Levels:: Manage sugar levels if you are a diabetic to help prevent fluid levels in the eyes from increasing, which causes swelling in the eyes.


How Can Oscar Wylee Help You Prevent Keratoconjunctivitis?
Oscar Wylee can help you prevent keratoconjunctivitis by providing comprehensive eye tests that can assist with assessing different parts of the eye. This will help ensure your eyes and vision are healthy. Oscar Wylee is an optical eyewear company that offers both prescription and non-prescription eyewear as well as primary eyecare and eye health services.
What is the Difference between Keratoconjunctivitis and Conjunctivitis?
The difference between keratoconjunctivitis and conjunctivitis is the specific region of the eye that is inflamed. Keratoconjunctivitis refers to the inflammation of both the cornea and conjunctiva while conjunctivitis involves the inflammation of just the conjunctiva. Conjunctivitis and keratoconjunctivitis present the same symptoms and have the same causes, keratoconjunctivitis is simply when you have conjunctivitis and keratitis.
What is the Difference Between Keratoconjunctivitis and Keratitis?
The difference between keratoconjunctivitis and keratitis is where the inflammation occurs. Keratoconjunctivitis affects the cornea and conjunctivitis and keratitis affects the cornea. Keratoconjunctivitis and keratitis are not very different as keratoconjunctivitis is when you have both keratitis as well as conjunctivitis.



